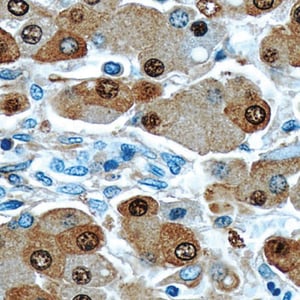
 Aside from tissue biopsy, cytology serves as an indispensable tool in screening and diagnosing cancer. In this technique, a cytological material is obtained from the patient, spread onto glass slides for microscopic examination, stained, screened for abnormalities and assessed prior to the issuance of a final report. Cytology differs from histology in that the sample usually consists of a suspension of cells whereas histology samples are usually sections of actual tissue. For example; a Gill’s hematoxylin single strength formulation would be much better suited for cytology, whereas a triple strength formulation would be better for tissue sections.
Aside from tissue biopsy, cytology serves as an indispensable tool in screening and diagnosing cancer. In this technique, a cytological material is obtained from the patient, spread onto glass slides for microscopic examination, stained, screened for abnormalities and assessed prior to the issuance of a final report. Cytology differs from histology in that the sample usually consists of a suspension of cells whereas histology samples are usually sections of actual tissue. For example; a Gill’s hematoxylin single strength formulation would be much better suited for cytology, whereas a triple strength formulation would be better for tissue sections.
Cytology examinations can be performed using the following specimen:
- Body fluids including urine, sputum or phlegm, cerebrospinal fluid (CSF), pleural fluid, pericardial fluid and ascetic or peritoneal fluid
- Cells that are scraped or brushed from the tissue or organ being tested (e.g., cells from the cervix, esophagus, stomach, bronchi and mouth)
- Palpable and non-palpable lesions
Cytological samples from palpable and non-palpable lesions from the area of interest can be obtained through a technique known as fine needle aspiration or FNA. Basically, this technique uses a fine needle (usually a 21-25 French gauge needle) to aspirate cellular material from the lesion and use it as a basis for making a diagnosis.
Processing Cytology Materials
In preparing cytology specimen, the material is smeared on glass slides and dipped in a series of stains (Diff Quick, Romanowsky, Papanicolaou, Hematoxylin and Eosin stain) before being examined under the microscope. However, since body fluids are too diluted, they are concentrated first before staining. Samples are then analyzed by a pathologist.
As required by federal law, clinical slides are kept in the lab for at least five years. This means that should a patient require a second opinion from a different doctor, the same sample can still be used (provided there is enough material available). Cytological materials can be subjected to a number of ancillary studies including simple special stains, immunohistochemistry, flow cytometry, cytogenetic analysis, electron microscopy and molecular pathology studies.
Importance of Cytology
Cytological examinations have numerous applications. They can be used for:
- Cytological tests such as Pap smears serve as an effective screening tool since they can be used to detect abnormalities and other changes in the cervix which may develop into cervical cancer.
- Routine follow-up procedure. This technique is also used as routine follow-up procedure after an initial diagnosis. For example, patients who were previously diagnosed with pulmonary carcinoma may be required to provide sputum, bronchial brushings, discharge samples and body cavity fluids (e.g., pleural, peritoneal and CSF) during the follow-up period.
- Diagnostic test. Cytological examinations can help clinicians and pathologists reach a definitive diagnosis that can help them provide an effective treatment plan for the patient.
Cytology vs. Biopsy: Weighing the Differences
While cytology and biopsy can both be used to effectively and safely diagnose cancer, there is a world of difference between these two. Here are some of their major differences:
- Specimen used. Biopsy uses body tissues while cytological tests use cellular materials. The collection of cytological specimen is less invasive and does not even leave a scar. In addition, the procedure does not cause any significant discomfort to the patient and has extremely low risk of resulting in serious complications.
- Specimen collection for cytology tests costs less since the procedure is extremely simple. It usually does not require the use of general anesthesia or any elaborate equipment.
- Due to the invasiveness associated with biopsies, they are often not performed unless there is sufficient suspicion or risk of a certain condition. While cytological procedures can sometimes be less accurate, they are much more suited for screening in a preventative manner.
There may be times when biopsy results are more accurate. This usually happens when cytology collection does not provide representative specimens or does not provide an easily recognizable abnormality for testing. Cytology often relies on certain cells being dislodged from a tissue and then collected. Thus, it makes perfect sense for a biopsy of that specific tissue to be much more accurate and informative than using the fluid that surrounds it. Cytology also fails to provide any structural information about how the cells are arranged within a tissue - something that is often useful when looking at early stages of tumorigenesis.
However, diseases such as cancer are known for having a prognosis that is directly related to the stage when it was diagnosed. Many cancer forms known for having poor prognosis, such as colon or prostate are also associated with late detection. While taking biopsies without a certain degree of suspicion of a condition is not advisable, this is where cytology shines. Procedures such as pap-smears are routinely used as to screen patients in a preventative manner. Until now, many of these routine checkup procedures where based on visual input as is the case for colonoscopies. However, advances in immunology and other diagnostic procedures are leading to less invasive procedures that have the potential to detect aberrances before the human eye can. Making screening procedures less invasive is a very important goal since it could lead to more frequent checkups and thus earlier diagnosis.
Related Blogs
Key Differences of H&E and Special Stains for Immunohistochemistry