Vaccines are undoubtedly one of the greatest turning points not only in the history of medicine and biomedical technology but also in the history of mankind. Historical evidence demonstrates that vaccination was performed in some form in ancient times, even before anything was known about the existence of the immune system. Vaccines have saved millions and millions of lives; mass vaccination has resulted in the eradication of diseases like smallpox and polio (almost at the brink of eradication) and made many other lethal pathogenic diseases like diphtheria, rabies, tuberculosis etc highly preventable. According to one report by WHO, vaccines saved more than 10 million human lives between 2010 and 2015 alone, and millions of more lives were prevented from severe illness because of mass vaccinations. The excitement surrounding the vaccines has been immense, be it governments, research organizations, pharmaceutical companies or general masses, everyone wants a safe vaccine for diseases that continue to haunt mankind despite the highly effective chemotherapeutic agents. It makes sense, prevention is better than cure!! Vaccines exactly do that.
The job of a vaccine is to ‘train’ the immune system to identify a pathogen so that on encountering the real threat (pathogen) immune system is well prepared to launch its attack on the invader. Very often, a vaccine is a modified pathogen/microbe (often a weakened or attenuated form of a pathogen) or even a part of the pathogen that closely mimics the real pathogen in molecular details but lacks the virulence and hence cannot cause disease. The advent of recombinant gene (gene-product) technology made subunit vaccines possible, eliminating the need to culture and produce non-virulent forms of pathogen required for vaccination at large scale. Subunit vaccines are small parts of a whole pathogen, for example, capsid proteins of certain viruses have been used to immunize against them. For a vaccine to be effective, it should elicit a robust immune response and produce long-lived immune memory. Moreover, the immunogen which does this should not persist forever in the body and be cleared from the system soon.
Why messenger RNA?
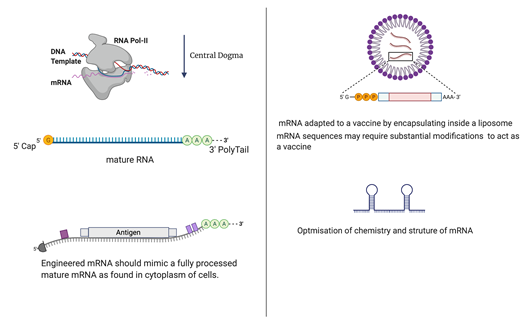
Messenger RNA plays a central role by acting as a template on which the polypeptide synthesis on ribosome occurs. Thus, it plays a central role in the relay of information from DNA to proteins. Eukaryotic mRNAs are more complicated than their prokaryotic counterparts. They have a cap on their 5’ terminus and a poly-A tail on their 3’ terminus. They can also undergo editing by splicing some parts and recombining them later to generate messenger RNAs of varied information and properties.
Messenger RNA is an inherently unstable molecule, it is degraded rapidly ex-vivo, even inside cells it has a transient existence. Moreover, mRNA is highly immunogenic and activates the innate immune system. And as if it all this was not enough; the mRNA molecule is also not readily taken up by the cells. What then makes messenger RNA, a molecule of choice for future vaccines?
The answer is both simple and complex, messenger RNA (mRNA) is a non-infectious, non-integrating molecule. mRNA can be optimized to express any protein inside cells. Not only this but mRNA can be engineered to express only in certain cells and not in others by engineering non-coding regions of mRNA. Thus, an injectable mRNA can closely mimic the natural infection where an intracellular pathogen produces proteins within certain cells inside the body of a host. On successful internalization, it can be exploited to express any protein to the desired level, its expression and half-life can be regulated by altering its UTR regions. Speaking in terms of production, production of a messenger RNA molecule is relatively inexpensive and easily scalable compared to protein-subunit vaccines or inactivated vaccines.
Despite all the promising features that messenger RNA offers, development of messenger RNA technology for a vaccine wasn’t easy and has been a long journey of failures and fortitude of gritty scientists to make it a reality. Some critical bottleneck issues that had to be overcome are as follows.
Stability and delivery: Messenger-RNAs are vulnerable molecules; scientists have found ways to improve the in vivo stability by engineering the UTRs. A messenger RNA to be delivered as a vaccine must be engineered to mimic a fully processed mature mRNA molecule with a 5’cap and a 3’poly A tail. Naked extracellular mRNA is quickly degraded by extracellular RNases, therefore scientists had to find ways to facilitate cellular uptake of mRNA molecules and protect them from degradation. Formulations that employ cationic polymers, liposomes or nanoparticles have been most successful in the successful delivery of mRNA into the cells.
A lot of research has gone into making it possible to successfully transfect cells with exogenous mRNA, a basic requirement for mRNA vaccines.
Dodging the immune system: Our innate immune systems have evolved to recognize free extracellular mRNA molecule as a potential viral threat and this may lead to undesired inflammatory activity when mRNA vaccine is administered. Scientists found that uridine is responsible for stimulating RNA receptors of the innate immune system, they have modified chemistry of mRNA by substitution of uridine with chemically modified bases such as pseudo-uridine and 1-methylpseudouridine. This has substantially suppressed the immunostimulatory action of mRNA. At the same time modification with chemically modified bases has resulted in improved expression of the protein by internalized mRNA.
Optimization for protein expression. The translation is an incredibly complex process, injecting a foreign messenger RNA to bring about protein expression may not always result in most fruitful protein expression, very often, without necessary intervention, the protein is expressed in low yields. Often the messenger RNA molecule requires engineering to enable it to adopt a favourable secondary structure which facilitates an efficient translation on ribosomes. Similarly, coding part of a messenger RNA sequence may require considerable codon optimization to facilitate an optimal expression of a protein in cells.
Needless to say, it anymore, mRNA technology for vaccines is going to be the technology of the future because it is more effective, readily adaptable to any disease or molecular target and allows for a fine regulation not possible with conventional vaccine platforms. Not just that, the small cost to make mRNA molecules and potential for scalable production will make it the best choice for vaccine platforms. mRNA technology has not only trumped the vaccine game, but it is emerging as a pharmaceutic of future, mRNA can act like a drug and holds a great promise for conditions that require protein replacement therapies.