Recent advancements in immuno-oncology are bringing hope to millions of cancer patients worldwide. Also known as cancer immunotherapy, this type of biological therapy exploits the power of the body’s natural defenses in fighting cancer in a safer and more effective way.
What is immune-oncology and how does it work?
In immuno-oncology, the patient’s immune system is stimulated or modified to improve its natural ability in fighting cancer while minimize toxicities. Despite the fact that the immune system naturally seeks, attacks, and destroys abnormal cells and other foreign bodies, there are times when cancer cells escape detection.
This usually happens when there are certain genetic changes in the cancer cells or when their surface is coated with certain proteins. The immune system may also fail to spot these anomalies when the cancer cells alter the healthy cells surrounding the tumor, making them virtually invisible to the patrolling immune cells.
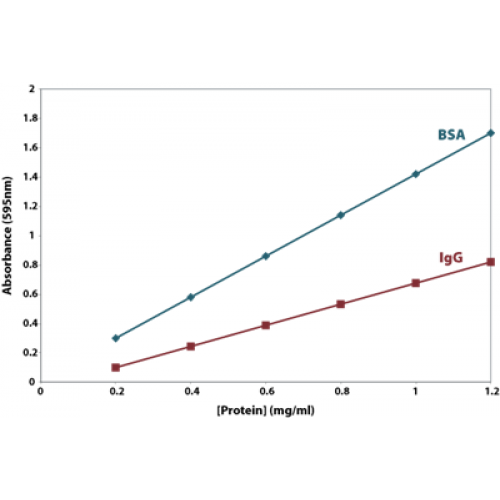
Cancer immunotherapy is based on the fact that the proteins or other macromolecules found on the cancer cells’ surface can be detected and bound by the antibody proteins of the immune system. Normal antibodies may work in binding external pathogens, but modified immunotherapy antibodies are more effective in identifying and binding tumor antigens.
What are the main types of cancer immunotherapies?
Immuno-oncology therapies can be generally classified as active or passive. Active immunotherapy specifically targets and destroys cancer cells by identifying their distinct markers (antigens), while passive immunotherapy works by enhancing the immune system’s ability to attack and destroy cancer cells.
Active cellular immunotherapy may include the following:
- Dendritic cell therapy. This works by activating the dendritic cells through vaccination (sipuleucel-T for prostate cancer, TVEC for melanoma). Upon activation, the dendritic cells present the tumor antigens to the lymphocytes which then primes them to recognize, react, and destroy other cells containing the identified antigens.
- T-cell transfer therapy. In T-cell immunotherapy, the T-cells are modified to boost their ability to target and destroy cancer cells. There are two types of T-cell transfer therapy: TIL (tumor-infiltrating lymphocytes) therapy and CAR-T cell therapy. Both treatments involve harvesting T-cells from the patient’s own tumor, cultivating them in the lab, and giving them back to the patient via injection. TIL therapy is effective for people with melanoma and other cancers such as cervical squamous cell carcinoma and cholangiocarcinoma, while CAR-T cell therapy is effective for blood, breast, and brain cancers.
- Monoclonal antibodies. Monoclonal or therapeutic antibodies are artificially-created antibodies designed to interact with specific targets on the cancer cells. Some of these antibodies are created to make the cancer cells more visible (e.g., rituximab), making them an easy target for the immune cells, while some are designed to stop the growth of cancer cells or cause them to self-destruct.
On the other hand, passive antibody therapy include the administration of the following treatments:
- Immune checkpoint inhibitors (CTLA-4, PD-1, and PD-L1). As the name suggests, these inhibitors work by blocking the immune checkpoints (the natural regulators of the immune pathway responsible for slowing down or reducing the immune response and preventing the immune system from attacking normal, healthy cells) to allow the immune cells to respond more strongly to cancer. Some of the most commonly used immune checkpoint inhibitors are Durvalumab (Imfinzi), ipilimumab (Yervoy), nivolumab (Opdivo), and pembrolizumab.
- Immune system modulators. Immune-modulating agents work by enhancing the body’s immune response to cancer and are used to treat advanced cancer. Some of the most commonly used immune system modulators are cytokines (interferons and interleukins), BCG, and immunomodulatory drugs (biological response modifiers) such as thalidomide, lenalidomide, pomalidomide, and imiquimod. The first three drugs work as angiogenesis inhibitors (prevent tumors from forming new blood vessels) while imiquimod helps by stimulating the cells to release cytokines.